

We recently had the chance to connect with Ricardo Johnson II and have shared our conversation below.
Good morning Ricardo, we’re so happy to have you here with us and we’d love to explore your story and how you think about life and legacy and so much more. So let’s start with a question we often ask: What are you most proud of building — that nobody sees?
Anyone who knows me knows that my greatest sense of pride comes from my children. Who they’ve become, what drives their daily lives, and the things they can do that I never taught them are all great sources of pride for me.
In my own life, the thing I’ve become most proud of, and maybe this is reflected in my first response to your question, is my abiding focus on what I am grateful for in each moment of the day. I don’t know if gratitude can be seen or not. I think it’s more likely that it’s felt, but my commitment to looking at each moment, whether it be light or heavy, and asking myself, “What is the blessing here?” has developed a great sense of perspective in me. I’m proud of the life gratitude has provided me and the world around me.
Can you briefly introduce yourself and share what makes you or your brand unique?
My name is Ricardo Johnson II. I am the founder and CEO of Muse Health and the Oasis Care Navigation Platform.
Muse Health is a health technology and population management company that builds and operates digital ecosystems designed to improve outcomes and reduce costs for payers, providers, employers, and consumers. Our model combines AI-powered care navigation, delivery, behavioral health, and peer support into a dynamic, interoperable platform that makes healthcare accessible, measurable, and culturally intelligent.
The U.S. healthcare system has always evolved in surprising and hard-to-predict ways. The changes that have occurred over the last 12 months are unprecedented in my professional experience. What currently has me excited is that our concept of “organic, authentic, and personal care”™ transcends market forces. Our commitment to whole-person care, delivering optimal outcomes, and reducing costs is embraced by payers, providers, and members with the same amount of enthusiasm.
Most organizations aspire to be nimble. The changes that we’ve made organizationally in the last 12 months have redefined my understanding of that word. As I sit here with you, I must admit that we are significantly better prepared to deliver on our mission than ever before, and we have this environment, balanced against our will to serve, to thank.
That statement is not meant to minimize the significant challenges that are being experienced in rural and urban areas, among the elderly and fixed-income individuals, and families with young children. Each is facing an uncertain future as it relates to healthcare, and we are here to act as an oasis in challenging times.
Appreciate your sharing that. Let’s talk about your life, growing up and some of topics and learnings around that. Who taught you the most about work?
Early in my life, I had an opportunity to watch my mother work a full-time job in Grand Rapids, Michigan, and then, on a weekly basis, drive to Bowie, Maryland, to teach classes at the end of the week and the weekend, only to be back in Grand Rapids for her full-time job on Monday.
So, examples of hard work have always been present in my life. But if you were to ask me who has taught me the most about work, I would have to say that spending the last 15 years watching Kevin Warren etch his name in the annals of sports business history is the example that has taught me the most about work.
Kevin comes to his daily work rooted in faith and in family. He has an extraordinary intellect, and yet if you were to ask me what the pillars of his excellence are, I would answer that no one outworks him, and that whatever he commits to do, he will do. That last statement is a promise or a threat, depending on who you are to him.
Most of my life, my ability gave me a false sense of achievement. I wasn’t the hardest worker; if a shortcut was available, I was never uncomfortable taking it, and the results were evident in my early career.
Kevin has, on occasion, generously referenced us as colleagues, when in fact I believe that he is, if you excuse the pun, in a league of his own. I, however, have been fortunate enough to learn from his example, and those lessons have manifested great blessings in my current endeavors.
If you could say one kind thing to your younger self, what would it be?
If I could say one kind thing to my younger self, I wouldn’t tell myself anything specific. My life has been filled with challenges, success and failure, pain and exhilaration, but what I feel most blessed about is that my life has been written in my own hand. So I would give myself no specifics. What has happened was meant to happen.
In the macro, what I would say is that many of the things I thought were very important, in fact, were not, and many of the things that I thought were unimportant were very important. I would invite myself to spend a little more time determining which is which.
Alright, so if you are open to it, let’s explore some philosophical questions that touch on your values and worldview. How do you differentiate between fads and real foundational shifts?
Thank you for this question. People hear “platform” or “med tech” and their eyes roll, and for good reason. OCNP isn’t another health tech fad; it’s a structural shift in how care is engaged, delivered, experienced, and financed.
In a marketplace flooded with tech that tells us what happened to a population they have never met last month or last year, OCNP was built to communicate to each stakeholder and personalize the experience of what is happening now and why. Connecting every layer of healthcare into one coordinated system, care navigation, AI intelligence, telehealth, wearables, peer support, and actuarial analytics, it’s the foundation, not an accessory.
Fads are revealed by results, or more specifically, poor results. OCNP sustains impact through robust technical infrastructure and is supported by 18,500 regionally deployed care navigators who are selected by the user as someone from their community, increasing the chances that the member will be understood. These are people, not algorithms. It’s live within payers like Allstate Health and BCBS, and extended through international programs with Beyond Activ and Purpose Brands’ Anytime Fitness and our Muse Mirror network. Our ecosystem’s reach makes it a core utility for payers and employers, not another app competing for downloads.
The platform’s intelligence engine doesn’t wait for claims or crises. It predicts risk, triggers intervention, and measures outcomes in real time, creating a closed feedback loop that turns data into daily action. Its compliance framework (HIPAA, GDPR, SOC 2) and zero-trust architecture give payers and providers the security foundation they require to operate at scale.
Culturally, OCNP is designed for empathy. Its peer support communities, recognition systems, and multilingual experience make care both personal and sustainable. Financially, it’s built around value-based care economics, aligning member outcomes with payer incentives.
In short, OCNP isn’t another app chasing attention. It’s the operating system for modern healthcare, turning fragmentation into coordination, transactions into relationships, and data into human outcomes.
Before we go, we’d love to hear your thoughts on some longer-run, legacy type questions. When have you had to bet the company?
I am a business owner, so every day is a calculated gamble. In the broader scope of your question, recently a lot has been made of the timing of our Oasis Care Navigation Platform (OCNP) pivot, but candidly, it started as something a lot simpler: our clients told us the system was broken, we listened, and we bet on people instead of technology.
At that point, we had already proven that we could build technology that connects, measures, and improves lives. The gamble involved whether we could actually bend the healthcare curve, not by adding another platform, but by providing interoperability to assist human-to-human or peer-to-peer interaction in something as fundamental as your next doctor’s appointment.
So many of these platforms are keys in search of locks. We spent years with the locks and then built a master key.
You know, the gamble we made with OCNP was believing that interoperability, systems integrity, and human connection could actually coexist, and that if they did, the return on investment would show up for all of the stakeholders.
As I said, we built the key after examining the locks. That key is actionable, real-time data, and not just for data’s sake. We were aligning the space between the data, that moment when a person makes a choice about their health, when a hospital tries to prevent an unnecessary readmission, or when a payer has to decide whether an outcome is worth the cost.
That’s where the real value lives.
Interoperability was our first unlock. Hospitals and payers have been drowning in fragmented data for years, labs that don’t talk to claims, EHRs that don’t sync with remote monitoring, disconnected point solutions that force clinicians to guess. The result? Billions lost annually from redundant tests, missed follow-ups, and avoidable readmissions. When you connect those dots through a human-first, dynamic, interoperable system, you start to see efficiencies that look good on a spreadsheet, lowering costs, and more importantly, saving lives.
Data liquidity alone doesn’t change behavior. People do. That’s why we designed OCNP as a human-first and human-last system, so members could select their own peer navigators, someone from their part of the country that they trust, someone who understands their background and their challenges. That human connection turns information into motivation. When members feel seen and supported, they actually follow care plans, show up to appointments, and engage with their own data. That’s how adherence becomes ROI.
Now, the integrity piece, the FWA&I layer. This is what makes all of this sustainable. As you bring data from multiple systems together, you also introduce risk: duplicate claims, false positives, and overbilling. By building integrity checks directly into the system, we protect both payers and providers from leakage and unnecessary spend. Our platform matriculates compliance to credibility.
From the payer’s side, ROI shows up in reduced utilization, fewer avoidable ER visits, fewer duplicative tests, and tighter chronic condition management. We’ve seen double-digit reductions in some models, and when you scale that across a population, it’s millions saved.
For hospitals, the return looks different but just as real. Better interoperability means shorter lengths of stay, smoother discharge coordination, and fewer readmissions, all of which drive margin back into care instead of waste. It’s also about reputation: better outcomes, higher quality scores, and stronger performance in value-based contracts.
At the heart of our platform are our members. Their ROI is personal. I recently spent half a day in an ER with my mother. The time sitting in an ER, the stress we carried trying to navigate a maze of disconnected systems, reminded me how important our systems are.
So yes, we made a bet. We bet that interoperability would create trust between systems, that FWA&I would create trust in the numbers, and that peer navigation would create trust between people. That combination, technology, integrity, and humanity is what makes the OCNP model work. It’s not a gamble anymore; it’s proof that when everyone’s ROI aligns, the whole system wins.
Contact Info:
- Website: https://oasiscnp.com
- Instagram: @mymusehealth
- Linkedin: https://www.linkedin.com/
- Youtube: @My.Muse.Health




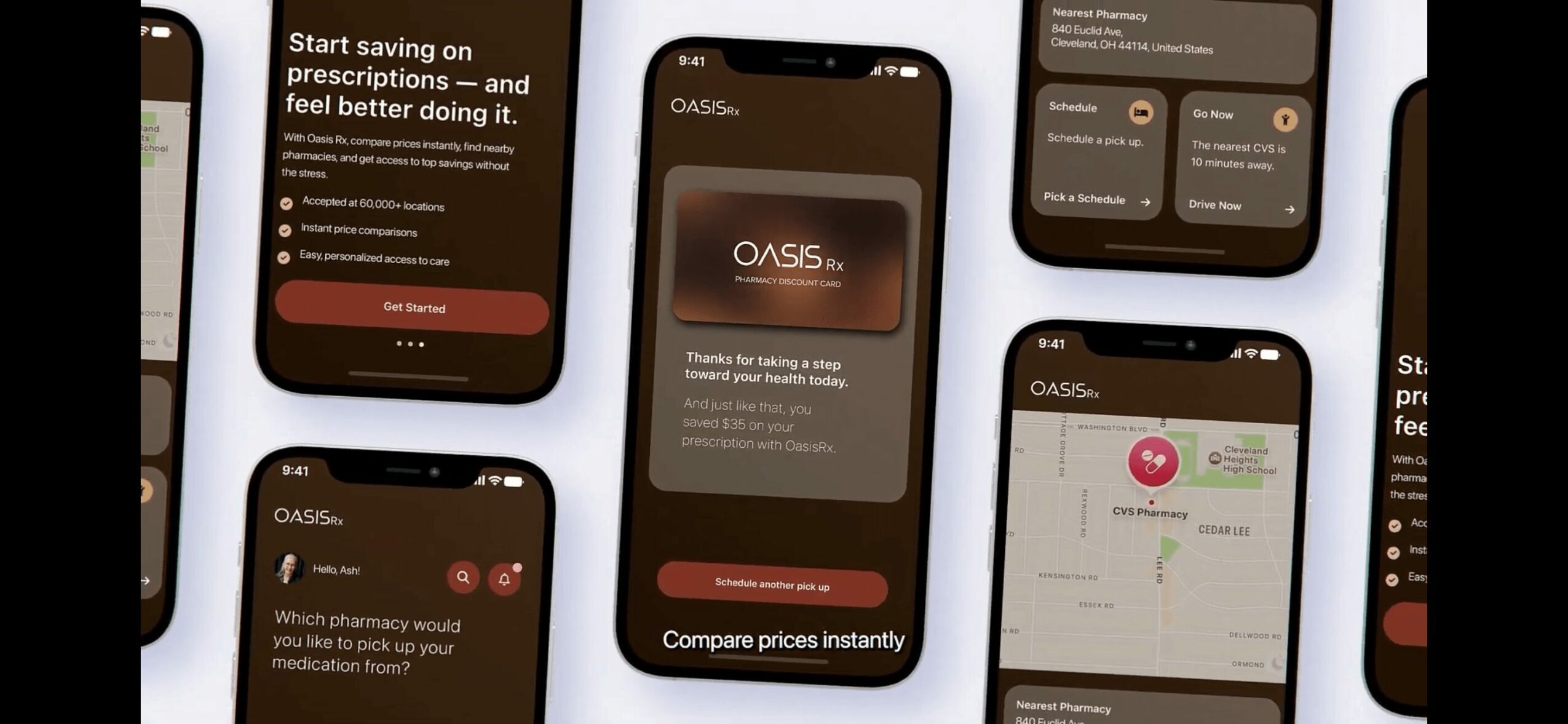
Image Credits
Muse Health’s CEO, Ricardo Johnson II and the Chicago Bears’ President and CEO Kevin Warren










